AHCCCS Member Eligibility Redetermination Update
During the pandemic, the Arizona Healthcare Cost Containment System (AHCCCS) was not allowed to remove anyone from Medicaid rolls. In April, AHCCCS began to re-determine everyone’s eligibility and will continue through March 2024. Members who are determined to be ineligible, either because their incomes are too high or lack of response to requests to update information, will be disenrolled.
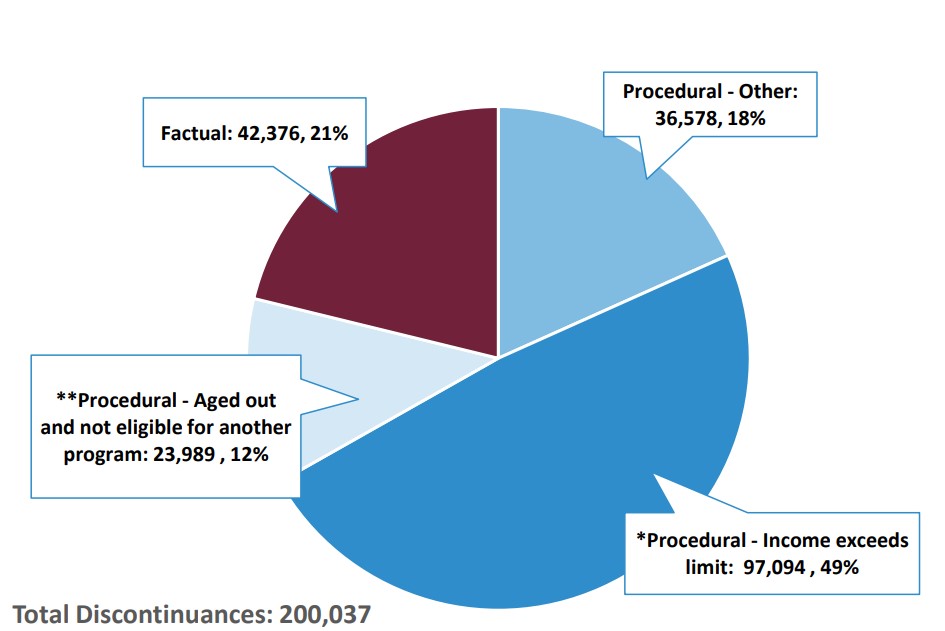
To date, 200,037 members have been dropped, and two thirds are due to some type of procedural problem. Anyone who has been notified that they were disenrolled for procedural reasons has 90 days to submit a renewal form that can restore their coverage without filling out a completely new application. To view the full AHCCCS Dashboard, click here.
Anyone who wants more information about affordable health insurance can go to Cover Arizona at www.coveraz.org where they can get more information about insurance options and arrange to speak to an insurance navigator for free.
Total Renewal Discontinuances Factual vs. Procedural
This data reflects renewal progress from April 2023 to current